 ASK THE EXPERT
ASK THE EXPERT
BMC : Prof. Van Meerbeek, how have bonding agents changed and advanced since you first began studying them?
Prof. Van Meerbeek : I believe that the great progress dental adhesive technology underwent in the last thirty years, and bonding agents in particular, have had a large impact on the field of dentistry, particularly restorative dentistry, of course. Many of the current restorative dental procedures make use of adhesive materials and techniques, and have advanced greatly as compared to when I wrote my PhD dissertation more than two decades ago on the topic of adhesion to dentin. Adhesion to enamel is, of course, relatively easy to achieve in comparison to adhesion to dentin, and when I first started researching this topic, I was limited to conducting clinical trials in which we were confronted with a relatively high number of restoration losses at short term. I was lucky to have been able to follow from the first row the fast advancement dental bonding has made, as having conducted research in this field now for nearly thirty years.
At a certain point, the research community started to realise that there is a smear layer in between that is created through cavity preparation, and that this layer interferes with bonding; if you want to achieve successful micromechanical and chemical bonding to the substrate, you first need to do something with this bond-interfering smear layer.
After this, we entered the era of conditioners and primers. In the past, the restorative community had been a little bit afraid of using phosphoric acid due to its potential for pulp irritation. More and more, however, dental professionals began to use etchants with this chemical in them, as well as primers that effectively promoted bonding between the adhesive resin and dentin. While having reached excellent bonding performance with multi-step adhesives in the laboratory, as also was later confirmed in clinical studies, further design and development of adhesive materials next focused towards simplification and shortening of bonding procedures.
Out of this, two kind of adhesives making use of two different bonding modes essentially arose: the etch-and-rinse adhesives1 and the self-etch (or etch-and-dry) adhesives2. The newest generation of universal adhesives now enables dental practitioners to choose which of the two bonding modes to apply with one single adhesive formulation.
What is your opinion regarding the current generation of universal adhesive solutions?
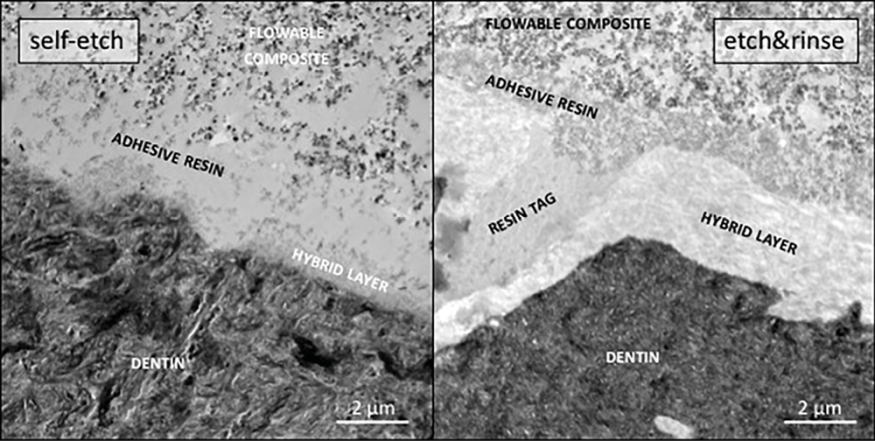
I think that this generation is very good (fig. 1), but that they are (still) not always as good as the more traditional and considered gold-standard two-step self-etch and three-step etch-and-rinse adhesives when it comes to their intrinsic bonding potential to dental tissue. However, I do see it as very positive that many of these universal adhesives integrate the 10-MDP monomer, which should be considered as one of the best functional monomers available today, though this unique monomer needs to be present at a sufficiently high concentration and purity level.
The 10-MDP monomer is, generally speaking, excellent at bonding to zirconia as well. Universal adhesives have indeed also been claimed to be indicated as part of adhesive luting workflows to bond semi-direct/indirect restorations to tooth structure. When it comes to bonding to different kinds of ceramic as well as resin-based composite restorative materials, it is always helpful to know which universal adhesives contain silane and are claimed to no longer need further (pre-)treatment of the restoration. This has the advantages of lower technique sensitivity and fewer procedural steps – provided that it does, of course, work. There is current scientific evidence that silane incorporated in today’s acidic aqueous universal adhesives is however insufficiently stable. Fortunately, research is underway to develop new universal adhesives that contain other silanes with higher stability in acidic aqueous solutions.
Overall, I believe that a universal restoration primer that contains a high concentration of silane along with 10-MDP in an ethanol (not water) solution is still more effective than many universal adhesives for bonding to restorative materials, since these universal adhesives contain many other ingredients that create a kind of competition within the material to reach and interact with the substrate surface, leading to lesser bonds.
Another somewhat neglected shortcoming of universal adhesives, as was also noted for the previous generation of one-step (self-etch) adhesives, is their thin film thickness and relatively high hydrophilicity, promoting water uptake and hence making them sensitive to hydrolytic degradation. In this light, it’s important to note that a viscous and hydrophobic flowable composite, when applied on top of a universal adhesive, can make up for this shortcoming somewhat and allow for durable bonding to take place.
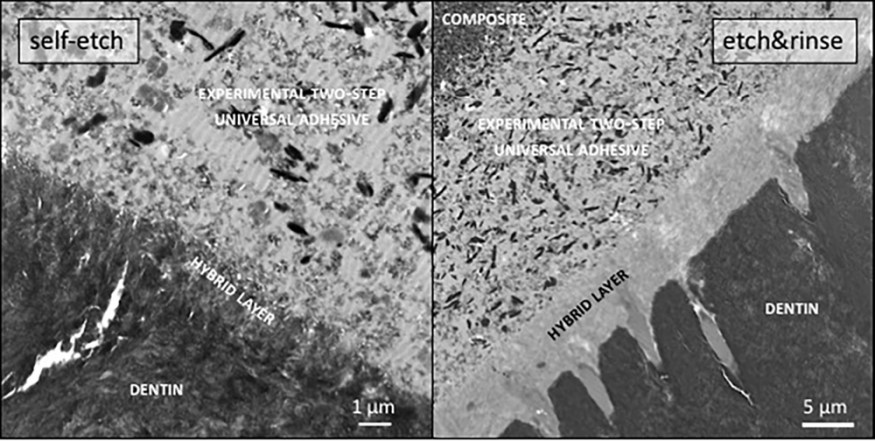
We actually currently work on the development of a two-step universal adhesive (fig. 2), which today does not exist and will be applicable in both etch-and-rinse and self-etch bonding mode, this to compensate for the inherent thin film-thickness shortcoming of today’s universal adhesive generation. The separate application of a well-polymerizing, hydrophobic and low water-absorbing adhesive3 following a 10-MDP primer in a two-step application procedure will better seal the adhesive interface against hydrolytic bond-degradation effects, while at the same time provide a thicker film thickness with interfacial stress-absorbing potential4. While involving a two-step application procedure (three-step application procedure following the optional etch-and-rinse bonding mode), this multi-step bonding mode should not necessarily be considered as less user-friendly5 or more time consuming, as this thick film-thickness adhesive incorporates the function of the flowable composite, which no longer is needed to be additionally applied. Today, clinical routines indeed often involve the application of flowable composite on top of thin film-thickness adhesives to stabilize the interface, while also improving marginal adaptation and tight sealing in critical cavity zones as the cervical box margin of posterior restorations. The new combined primer/adhesive resin universal adhesive will include the ‘flowable composite’ functionality, well realizing that hydrophobically sealed adhesive interfaces will most likely never be achievable with single-solution trade-off6 adhesives that would need to combine sufficient hydrophilicity for dentin-wetting67 purposes with high hydrophobicity upon polymerization to limit water uptake. Scientific research should correct current marketing that a price in terms of lower bond durability needs to be paid for simplified application procedures of dental adhesives.
Is the 10-MDP monomer crucial to the ultimate success of universal adhesives? Are there other factors that can influence this?
Well, it’s very clear that the 10-MDP monomer is one of the most effective monomers available, since it’s primary chemical binding potential to hydroxyapatite (fig. 3). It is important to stress that one may wrongly conclude that chemical binding will increase bond strength. Immediate bond strength should principally be attributed to micro-mechanical interlocking, while chemical binding as the most intimate contact atoms and molecules can mutually have, will contribute to bond durability or in other words will prevent/limit bond-strength reduction upon aging.
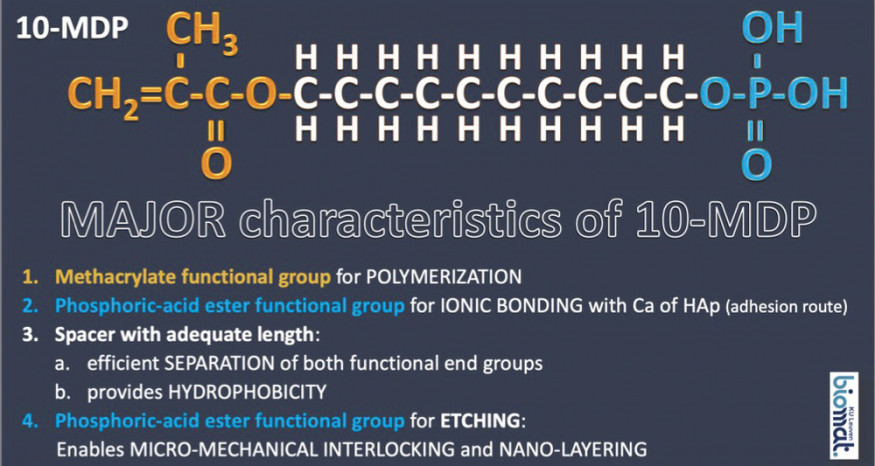
Although most, not all, commercial universal adhesives contain 10-MDP as functional monomer, there remain differences in bonding performance as there are significant differences in the 10-MDP purity and concentration levels between these products, factors that are also affected by whether or not the monomer is synthesised by the company itself or whether this process is outsourced. Essentially, a universal adhesive that contains a high concentration of very pure 10-MDP monomer should perform the best.
Are there any specific advantages that self-etch adhesives possess?
The biggest advantage is that self-etch adhesives don’t remove all hydroxyapatite and minerals present in dentin and so keep the weaker dentinal collagen protected. Phosphoric-acid etching results in relatively deep and complete demineralisation with collagen exposure, making the bond more prone to degradation, also to the so-called enzymatic bio-degradation, while the latter bond-degradation mechanism should be regarded as much less determining than water sorption and hydrolytic degradation effects. Partially maintaining minerals around collagen following a mild self-etch bonding mode additionally allows for strong ionic bond formation to take place when the adhesive in particular contains the functional monomer 10-MDP. As mentioned before, one should be aware that while chemical binding doesn’t necessarily lead to higher bond strength, it can create better long-term bond durability. That’s why we think that self-etch adhesives or universal adhesives employed in self-etch mode are the current references to stably bond to dentin.
What do you see as the next step in adhesive dentistry?
One possibility is to reduce the number of steps in the adhesion process with the final goal of having self-adhering restorative materials. There have been developments in this direction, studies and commercial products, though the products haven’t always proved to be very effective and their bond durability is unclear. Now, however, there are newer materials coming to market that can be used without any pre-treatment claimed necessary. Their clinical effectiveness nevertheless still needs to be proven and guaranteed before such self-adhering restorative materials could be used as true amalgam alternatives in routine dental practice. Manufacturers should therefore be encouraged to support long-term clinical research on their innovative self-adhering restorative material developments.
Another possibility and current R&D hype is the development of ‘bioactive’ adhesives. Many dental researchers, and many companies, want adhesives to not only deliver good bonding performance, but also to have certain therapeutic benefits. What, exactly, a bioactive adhesive is depends on who you’re talking to. Some researchers believe that they should have anti-bacterial qualities, whereas others state that remineralisation of dentin and pulpal cell interaction are needed to qualify for the term bioactive. We certainly need to look at if we can give these materials these additional properties, but under one condition: that the adhesive material does not lose any of its original bonding abilities. That is, in my opinion, the biggest challenge for the future of adhesive dentistry.
LEXIQUE
1. Etch-and-rinse adhesives : adhésifs mordançage et rinçage
2. Self-etch adhesives : systèmes auto-mordançants
3. Low water-absorbing adhesive : adhésif à faible absorption d’eau
4. Thicker film thickness with interfacial stress-absorbing potential : film plus épais avec un potentiel d’absorption
des contraintes à l’interface
5. Less user-friendly : moins facile d’utilisation
6. Trade-off : compromis
7. Wetting : mouillage











Commentaires